Bones are often thought of as strong, rigid structures that support the body throughout life. However, for many people, bones gradually lose their strength and resilience, becoming more and more brittle over time. This change may happen silently, without obvious symptoms, until a simple fall or minor injury leads to a fracture that seems disproportionate to the accident.
The question “Why do bones become more and more brittle?” is one of the most common concerns in bone health, especially among aging adults, cancer survivors, and individuals with chronic medical conditions. Bone brittleness is not a single disease—it is a condition that can result from aging, nutritional deficiencies, genetic disorders, medical treatments such as chemotherapy, and lifestyle factors.
In this article, we will explore:
- What it really means when bones become brittle
- Whether bones naturally become brittle with age
- What brittle bone disease is and how it differs from osteoporosis
- Whether chemotherapy can cause brittle bones
- How brittle bones are diagnosed, prevented, and treated
This guide is written using evidence-based medical knowledge and practical experience to help you understand bone fragility and take informed steps to protect your skeletal health.
As the years gracefully pass us by, our bodies embark on a remarkable journey filled with incredible transformations. However, amidst this captivating process lies an unfortunate reality – why do our bones become more and more brittle as we age? Enter the intriguing keyword: “osteoporosis.” Picture your skeleton as a magnificent architectural masterpiece, built upon a foundation of calcium and collagen fibers meticulously woven together.
What Is the Brittle Bone Disease?
Brittle bone disease is a genetic condition medically known as osteogenesis imperfecta (OI). It is caused by a defect in the production of collagen, a protein that gives bones their strength and flexibility. Because of this defect, bones are weaker than normal and can break easily, sometimes from minor injuries or even normal daily activities. The condition is usually present from birth and can range from mild forms with occasional fractures to severe forms that cause frequent breaks and bone deformities.
In addition to fragile bones, people with brittle bone disease may experience other symptoms such as short stature, bone curvature, loose joints, and a blue or gray tint to the whites of the eyes. Unlike osteoporosis, which typically develops later in life due to bone density loss, brittle bone disease is inherited and affects bone quality rather than just bone density. While there is no cure, treatment focuses on managing symptoms, preventing fractures, and improving quality of life through medical care, physical therapy, and lifestyle support.
Symptoms of Brittle Bone Disease
Brittle bone disease, also known as osteogenesis imperfecta (OI), can vary in severity, but common symptoms include:
- Frequent fractures: Bones break easily, often with little or no trauma.
- Bone deformities: Curved or misshapen bones may develop over time.
- Short stature: Individuals may be shorter than average due to bone growth issues.
- Loose joints and weak muscles: Increased flexibility in joints can affect stability.
- Blue or gray sclera: The whites of the eyes may appear bluish or grayish.
- Hearing loss: Some types of OI may affect the bones in the ear, leading to hearing problems.
- Dental issues: Brittle teeth or other dental abnormalities may occur.
Symptoms can range from mild to severe, and early diagnosis is important to manage fractures, support bone health, and improve quality of life.
Do Bones Become Brittle With Age?
Yes, bones do become more brittle with age, and this is one of the most common and well-documented causes of bone weakness. Aging affects bone health in several interconnected ways.
Why Bone Density Declines With Age
As people age, the body becomes less efficient at maintaining bone mass. Several biological changes contribute to this process:
- Reduced Calcium Absorption
The digestive system absorbs calcium less efficiently with age, even if dietary intake remains adequate. - Lower Vitamin D Levels
Aging skin produces less vitamin D from sunlight, which directly impacts calcium absorption and bone mineralization. - Hormonal Changes
- In women, estrogen levels drop sharply after menopause. Estrogen plays a critical role in slowing bone breakdown.
- In men, testosterone levels gradually decline, also contributing to bone loss.
- Reduced Physical Activity
Bones require mechanical stress to stay strong. With age, people often become less active, accelerating bone loss.
At What Age Do Bones Start Becoming Brittle?
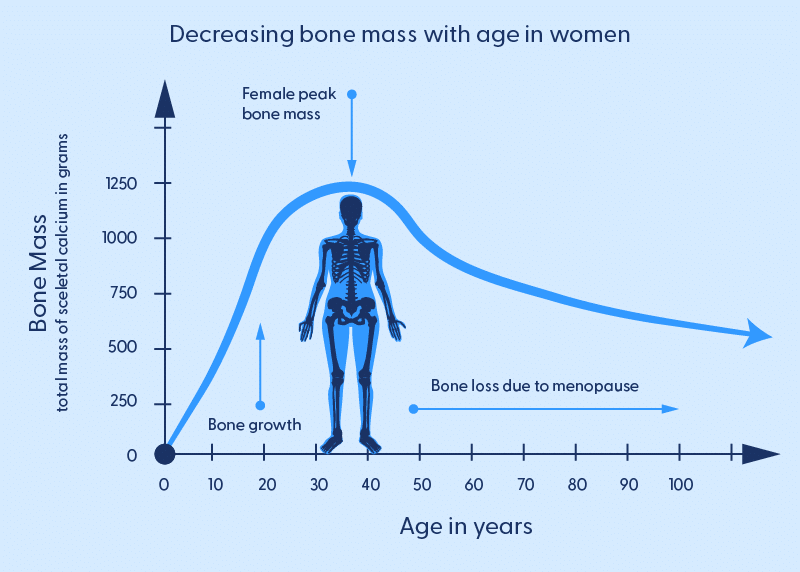
Bone mass typically peaks between the ages of 25 and 30. After this point, bone density slowly declines. For most people:
- Bone loss begins subtly in the 30s and 40s
- It accelerates after age 50
- Women experience faster bone loss after menopause
- Men usually experience bone brittleness later in life, but it still occurs
This gradual decline explains why fractures of the hip, spine, and wrist are far more common in older adults.
Signs That Your Bones May Be Weakening
Bone loss often progresses without symptoms until a fracture occurs. However, some warning signs may include:
- Fractures from minor falls or low-impact injuries
- Loss of height over time
- A stooped or hunched posture
- Chronic back pain due to spinal compression fractures
Early detection is crucial because bone loss can often be slowed or treated if identified in time.
Does Chemo Cause Brittle Bones?
Yes, chemotherapy can cause or worsen brittle bones, especially when treatment lasts for several months or is combined with other cancer therapies. Some chemotherapy drugs disrupt the normal bone remodeling process by slowing bone formation and increasing bone breakdown. Chemotherapy can also lead to side effects such as nausea, poor appetite, and fatigue, which may reduce calcium and vitamin D intake and limit physical activity—both essential for maintaining strong bones.
Additionally, chemotherapy is often used alongside treatments like steroids, hormone therapy, or radiation, all of which can further weaken bones. In some cases, chemotherapy may trigger early menopause in women or reduce testosterone levels in men, significantly increasing the risk of bone loss and fractures. While not all patients develop brittle bones, cancer patients and survivors have a higher risk and should consider bone density monitoring, proper nutrition, and medical guidance to protect their bone health.
Other Causes of Brittle Bones
Aging and medical treatments are not the only reasons bones become brittle. Other common causes include:
- Vitamin D deficiency, which impairs calcium absorption
- Calcium deficiency, leading to weaker bone structure
- Long-term steroid use, such as prednisone
- Autoimmune diseases, including rheumatoid arthritis
- Thyroid disorders, particularly hyperthyroidism
- Smoking, which reduces blood supply to bones
- Excessive alcohol consumption, which interferes with bone formation
These factors often act together, compounding bone loss over time.
How Are Brittle Bones Diagnosed?
Diagnosing brittle bones involves a combination of careful evaluation, medical tests, and imaging studies to understand the strength and condition of your bones. Each step provides essential information for accurate diagnosis and treatment planning.
1. Medical History Review
The first step in diagnosing brittle bones is a thorough review of your medical history. Doctors will ask about previous fractures, even those that occurred from minor injuries, as they may indicate underlying bone weakness. They will also inquire about family history of osteoporosis or genetic bone disorders, lifestyle habits such as diet, physical activity, smoking, and alcohol consumption, and any medications you take that could affect bone health, such as corticosteroids. This step helps identify risk factors and guides the need for further testing.
2. Physical Examination
A physical exam allows doctors to observe visible signs of bone fragility. They may look for bone deformities, changes in posture, curvature of the spine, or loss of height, which can suggest vertebral compression fractures. Joint flexibility and muscle strength may also be assessed to understand how bone weakness is affecting overall mobility and stability. These observations can provide early clues about conditions like osteoporosis or genetic brittle bone disorders.
3. Bone Density Test (DEXA Scan)
The DEXA scan (dual-energy X-ray absorptiometry) is the gold standard for measuring bone mineral density (BMD). During the scan, a low dose of X-rays passes through your bones to determine their density and strength. Results help categorize bone health as normal, osteopenic (mild bone loss), or osteoporotic (significant bone loss). This test is painless, non-invasive, and quick, typically taking only a few minutes, and is essential for evaluating fracture risk.
4. Blood Tests
Blood tests are used to uncover underlying factors contributing to bone fragility. Doctors often check calcium, vitamin D, phosphorus, and parathyroid hormone levels because deficiencies or imbalances can weaken bones. In some cases, tests for thyroid function, kidney function, or genetic markers are ordered, especially if a hereditary condition like brittle bone disease is suspected. These tests help identify treatable causes of bone weakness.
5. Additional Imaging Tests
In certain situations, X-rays, CT scans, or MRI may be used to detect existing fractures, bone deformities, or structural abnormalities that are not visible in a routine exam. These imaging studies provide detailed information about the severity of bone damage and guide treatment decisions.
Treatment Options for Brittle Bones
Treating brittle bones involves a combination of medical care, lifestyle adjustments, and supportive therapies to strengthen bones, reduce fracture risk, and improve overall skeletal health. The exact approach depends on the underlying cause, age, and overall health of the individual.
1. Medications to Strengthen Bones
Doctors may prescribe medications like bisphosphonates, which help slow bone loss and increase bone density. Other options include denosumab, teriparatide, or hormone therapies, especially for postmenopausal women or those with osteoporosis. These treatments help reduce the risk of fractures and improve bone strength over time.
2. Nutritional Support
A diet rich in calcium, vitamin D, magnesium, and protein is essential for bone repair and maintenance. Supplements may be recommended if dietary intake is insufficient. Proper nutrition ensures the body has the minerals necessary to maintain strong and healthy bones.
3. Exercise and Physical Therapy
Weight-bearing and resistance exercises, such as walking, jogging, or strength training, stimulate bone formation and improve muscle strength, which supports bone stability. Physical therapists can design personalized exercise programs that are safe and effective, especially for older adults or those recovering from fractures.
4. Lifestyle Modifications
Healthy habits are crucial in preventing further bone weakening. Avoiding smoking, limiting alcohol intake, maintaining a healthy weight, and practicing fall-prevention strategies can significantly reduce the risk of fractures.
5. Holistic Wellness Support
Integrating holistic care can further enhance bone health. Centres like The Family Wellness Centre (thefamilywellnesscentre.com.au
) offer services such as chiropractic care, postural assessments, nutritional guidance, and personalized wellness programs. These approaches help improve overall body alignment, reduce stress on bones and joints, and support long-term skeletal health.
6. Surgical Interventions (When Necessary)
In severe cases involving fractures, bone deformities, or osteoporosis-related complications, surgical options such as bone grafts, spinal stabilization, or hip replacement may be required to restore function and prevent further injury.
By combining medication, proper nutrition, exercise, lifestyle adjustments, and holistic wellness support, individuals with brittle bones can strengthen their skeletal system, reduce the risk of fractures, and maintain mobility and quality of life.
Contact us now
This hormonal imbalance further exacerbates the problem, leaving behind weakened structures that are frightfully susceptible to fractures at even the slightest provocation. So here we stand – captivated witnesses to this beguiling dance between time’s relentless march forward and our body’s struggle against its unyielding grip.
Frequently Asked Questions About Brittle Bones
1. Can brittle bones be reversed?
Brittle bones cannot usually be fully reversed, but strength can be improved and further loss slowed with proper nutrition, exercise, and medical treatments.
2. Are brittle bones hereditary?
Some forms, like osteogenesis imperfecta, are hereditary, while age-related bone loss is influenced by lifestyle, though family history can increase risk.
3. What vitamins and minerals help strengthen bones?
Key nutrients include calcium, vitamin D, magnesium, vitamin K2, and protein, which support bone strength and repair.
4. Can chemotherapy cause brittle bones?
Yes, chemotherapy can weaken bones by affecting bone remodeling and hormones; monitoring, nutrition, and exercise can help protect bone health.
5. How can I prevent brittle bones as I age?
Preventive steps include a calcium- and vitamin D-rich diet, weight-bearing exercises, avoiding smoking and excess alcohol, maintaining healthy weight, and seeking professional wellness support.
6. How are brittle bones diagnosed?
Diagnosis involves medical history, physical exams, DEXA scans, blood tests, and sometimes X-rays or MRI to assess bone strength and fracture risk.
Conclusion
Brittle bones are a common but serious condition that can affect people of all ages, caused by factors such as aging, genetic disorders, medical treatments, and lifestyle choices. Understanding the reasons behind bone fragility whether it’s age-related bone loss, brittle bone disease, or chemotherapy-related weakening is essential for taking proactive steps to maintain bone health. Early diagnosis, proper nutrition, regular exercise, and medical care play a critical role in preventing fractures and maintaining mobility.
Holistic approaches, like those offered by The Family Wellness Centre, can complement traditional treatments by improving posture, alignment, and overall musculoskeletal health, helping to reduce stress on bones and joints. By combining medical guidance, lifestyle adjustments, and supportive wellness programs, individuals can protect their bones, enhance strength, and preserve their independence and quality of life for years to come.